Adam Kay is Coming. And It Hurts.
Adam Kay is bringing his brutally funny, painfully honest show This Is Going to Hurt to New Zealand and Australia as part of the 2025 Comedy Festival.
We were given this book by one of our course participants. We laughed. We cried. And we were shaken.
Not as medical professionals, but as people who interact with the healthcare system, and as people who have had the immense privilege of hearing hundreds of stories from those working on the inside.
What Kay describes in his book isn’t satire. It’s reality, confirmed again and again in every Process Communication Model (PCM) workshop we run with healthcare professionals. These are the people who show up every day to keep the system running – and who often pay for it with their wellbeing, their relationships, and sometimes their health.
This post isn’t about Adam Kay’s tour. It’s about the strange realisation that the more the system hurts its people, the more its people go above and beyond to hold it together. And that’s what makes it so hard to fix.
Why Healthcare Keeps Going, Even When the System Fails
Recently, hundreds rallied outside Nelson Hospital, protesting staffing shortages and growing waitlists. We watched it unfold like so many other rallies before it: with deep compassion, and also confusion.
Because from the outside, it’s baffling: how has the system not collapsed already?
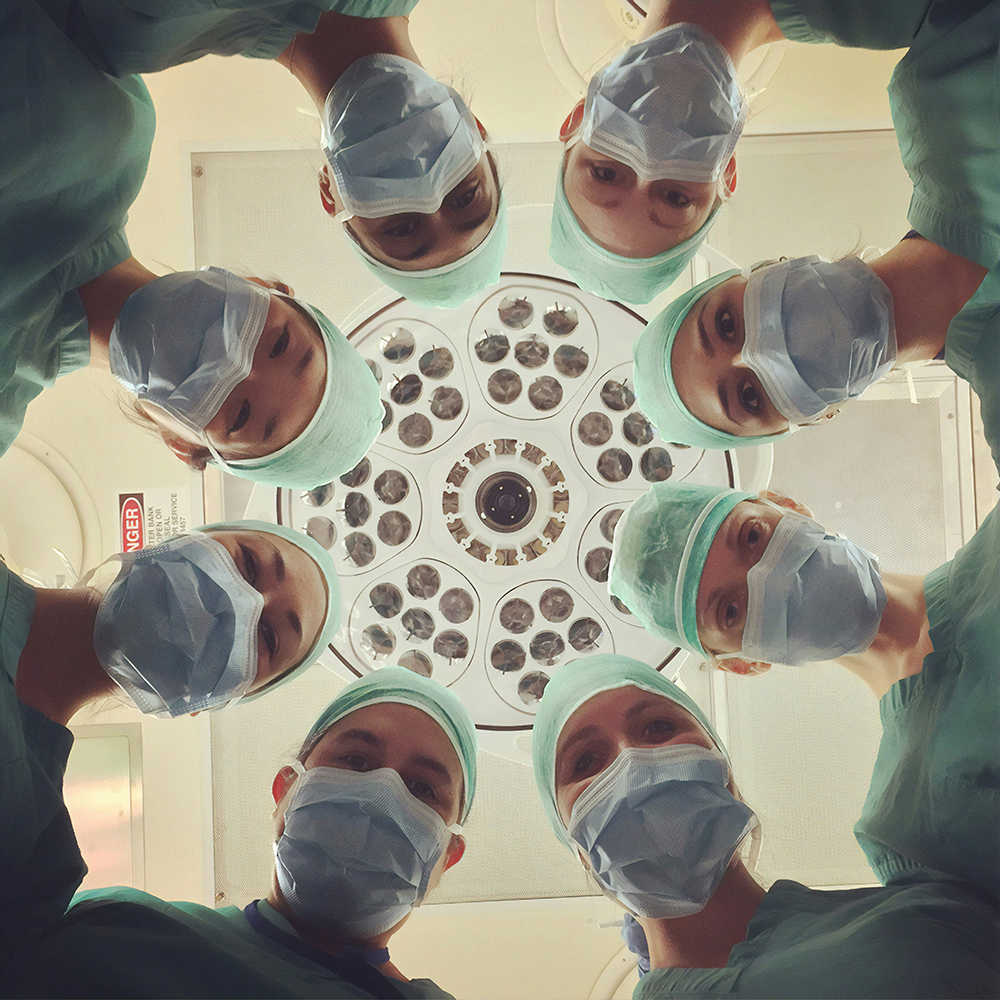
The answer is painfully simple. Because it’s held up by people who care. By doctors and nurses who continue to go the extra mile, even when they’re running on empty.
As Kay puts it:
“We can’t treat doctors and nurses as human beings—because if we did, we’d have to admit the system doesn’t work. And that’s not acceptable.”
In interviews, Kay has shared that after his book was published, countless doctors reached out to him saying:
“Until I read that bit in your book, I thought I was the first doctor who’d ever cried in the locker room.”
We hear versions of this all the time. In breaks. After sessions. Sometimes with tears. Often with laughter that doesn’t reach the eyes.
We’re often invited in as a kind of remedy. But what we really offer is a way to shift the system from reactive to responsive. PCM gives teams a shared language – not just for communication, but for care. It helps people recognise distress early, understand what’s driving it, and respond in ways that defuse tension instead of feeding it.
How Healthcare Leaders Build Trust (Not Just Systems)
Over the years, we’ve had the privilege of working with hundreds of healthcare professionals across levels, teams, and disciplines. What we’ve seen consistently is that the most effective leaders aren’t the ones with the best plans. They’re the ones who know how to connect.
Too often, healthcare rewards a narrow focus on accountability, delivery, and efficiency. And when that doesn’t work, it adds compassion and equity – but again, in policy terms, not human ones.
“Policies and procedures only work if we can connect as human beings.”
Connection isn’t something you switch on for special cases. It’s how trust is built, or lost, from the outset. And in a high-pressure environment, that window is short.
PCM is what allows professionals to make that connection in real time, with laser precision. It’s not theory. It’s not fluff. It’s a clinical-grade tool for psychological safety and communication.
We often say that PCM is like a stethoscope for human behaviour. It lets you tune into what’s really going on beneath the roles, the uniforms, the scripts. It helps you adjust your approach based on how someone is truly experiencing the moment, not just what they’re saying.
Preventing Disconnection in Healthcare Culture
In healthcare, everyone knows prevention is better – and cheaper – than treatment. It’s curious how rarely we apply that to the workplace.
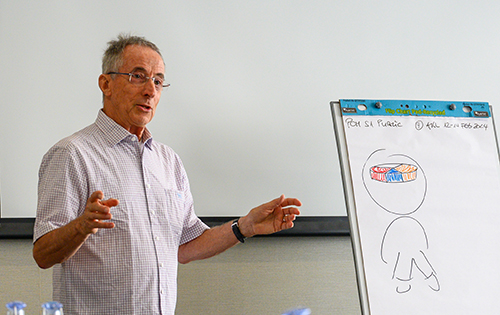
We often meet people at a crossroads. Sometimes they come into our public courses because they’ve been labelled as ‘having a problem’ or being ‘difficult to work with.’ Other times, it’s because team dynamics have broken down and communication has become strained.
But increasingly, we’re seeing something hopeful: people being referred to PCM before things go wrong.
From registrars preparing for surgical interviews, to team leads navigating challenging transitions, more and more professionals are being equipped with PCM early. This shift from remediation to preparation gives us hope.
One team shared a deceptively simple shift that made a big difference:
“Our meeting etiquette is always to connect first, and context comes later.”
It might sound small. But we’ve seen it change the entire tone of a team. Especially in systems dominated by Thinker and Persister values, where efficiency and detail are prized, and where emotional connection can be seen as “fluff.”
“Many of our workforce don’t work optimally because they are disengaged or disconnected. You can’t allow that to fester. One disengaged person can kill the morale of a whole team.”
PCM gives teams a practical way to re-engage. It’s not about telling people to care more—it’s about showing them how.
Why Emotional Intelligence Isn’t a Soft Skill in Healthcare
One of the most profound truths we’ve heard from leaders—though few dare say it out loud—is this:
“People bring baggage to work. Negative events in their private life affect their energy and performance. None of the usual leadership skills help people navigate that like PCM does.”
And this is exactly what Adam Kay writes about too:

But it is the source of care. The reason people show up. The reason the system hasn’t collapsed.
What If We Started with What’s Working?
So, as outsiders looking in, and as facilitators listening in, we’re left with this question:
What might change if we recognised connection with each individual as a core skill – not a soft one?
And what if, instead of only fixing what’s broken, we started by supporting what’s working: the people?
That’s not a solution. But it might be a start.
And if you’re wondering what that might look like in your team, your hospital, your training program, we’d love to share what we’ve seen work. Because there’s a way forward. And it doesn’t start with policy. It starts with people.
Want to learn the skills behind those shifts? Our PCM training courses are open to everyone in healthcare – practical, proven, and ready to use from day one.
FAQ: Supporting Healthcare Leaders and Teams
Q1: What is the Process Communication Model (PCM) in healthcare?
PCM helps healthcare professionals do what they were trained to do: connect with people. It gives language to the invisible: distress signals, emotional needs, and interpersonal blind spots. It’s about meeting people where they are, even in moments of pressure or crisis.
Q2: How can PCM reduce burnout in healthcare?
Burnout in healthcare doesn’t arise solely from long hours or heavy workloads—it often takes root when people feel disconnected: from their teams, from their sense of purpose, or from the support they need to thrive. Research highlights that factors like relationship breakdowns, misaligned values, and lack of recognition play a key role.
PCM provides a practical way for teams to understand and respond to the diverse motivational needs of individuals. By improving day-to-day communication and recognising early signs of stress, PCM helps foster stronger connections, a greater sense of belonging, and healthier team dynamics. It’s one part of a broader effort to create working environments where people feel seen, heard, and supported.
Q3: Who should use PCM in the healthcare system?
In a healthcare environment that’s increasingly complex and collaborative, effective communication isn’t just valuable—it’s foundational. PCM offers practical tools for anyone working in healthcare who wants to better understand their colleagues, build stronger teams, or improve interactions with patients. Whether you’re leading a department, mentoring new staff, or supporting patients and families in challenging moments, PCM can help you communicate more intentionally and adaptively..